Collective Trauma, Embodiment, and Community | Dr. Arielle Schwartz
Our Shared Hero’s Journey I invite you to think of collective trauma as a call to enter the transformational process of a hero’s journey. Collective trauma
Our Shared Hero’s Journey I invite you to think of collective trauma as a call to enter the transformational process of a hero’s journey. Collective trauma

Awakening to your Felt Sense Embodiment is as an active process of self-discovery that you renew and strengthen by repeatedly attending to your sensations, emotions,

A Restorative Reset Although rest is an integral part of our body’s rhythm, many of us have a complicated relationship to rest. That’s because our

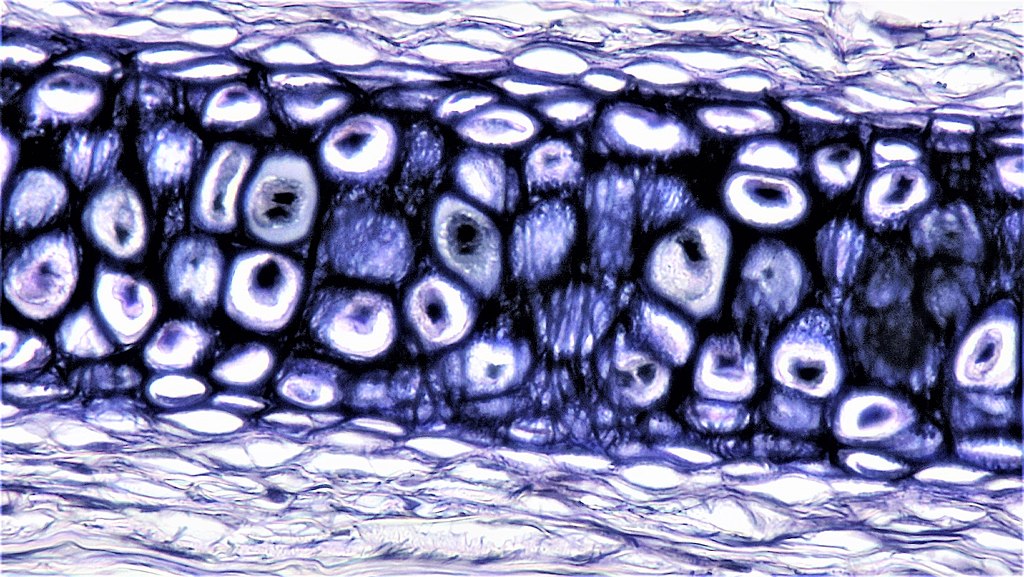
The Window to your Soul It is often said that the eyes are a window to your soul. Indeed, your eyes provide great insight into

A Backpacking Travelogue Alongside the ongoing weight of the global pandemic, another area of distress that is increasingly coming up for people is climate grief

A Sacred Pilgrimage Healing from trauma invites you to befriend your body; and this needs to occur at a pace that honors your unique needs.
A Podcast with Sounds True Recently, I had the honor to have a heartfelt conversation with Tami Simon with Sounds True, host of Insights at
Healing from the Inside Out Have you ever had a morning in which you wake up with a painful knot in your neck? What happened?