
Let Your Body Hold You
Immersive Polyvagal Practices for Trauma Recovery Let Your Body Heal You offers a strengths-based, embodied approach designed to meet the unique needs of anyone recovering

Immersive Polyvagal Practices for Trauma Recovery Let Your Body Heal You offers a strengths-based, embodied approach designed to meet the unique needs of anyone recovering
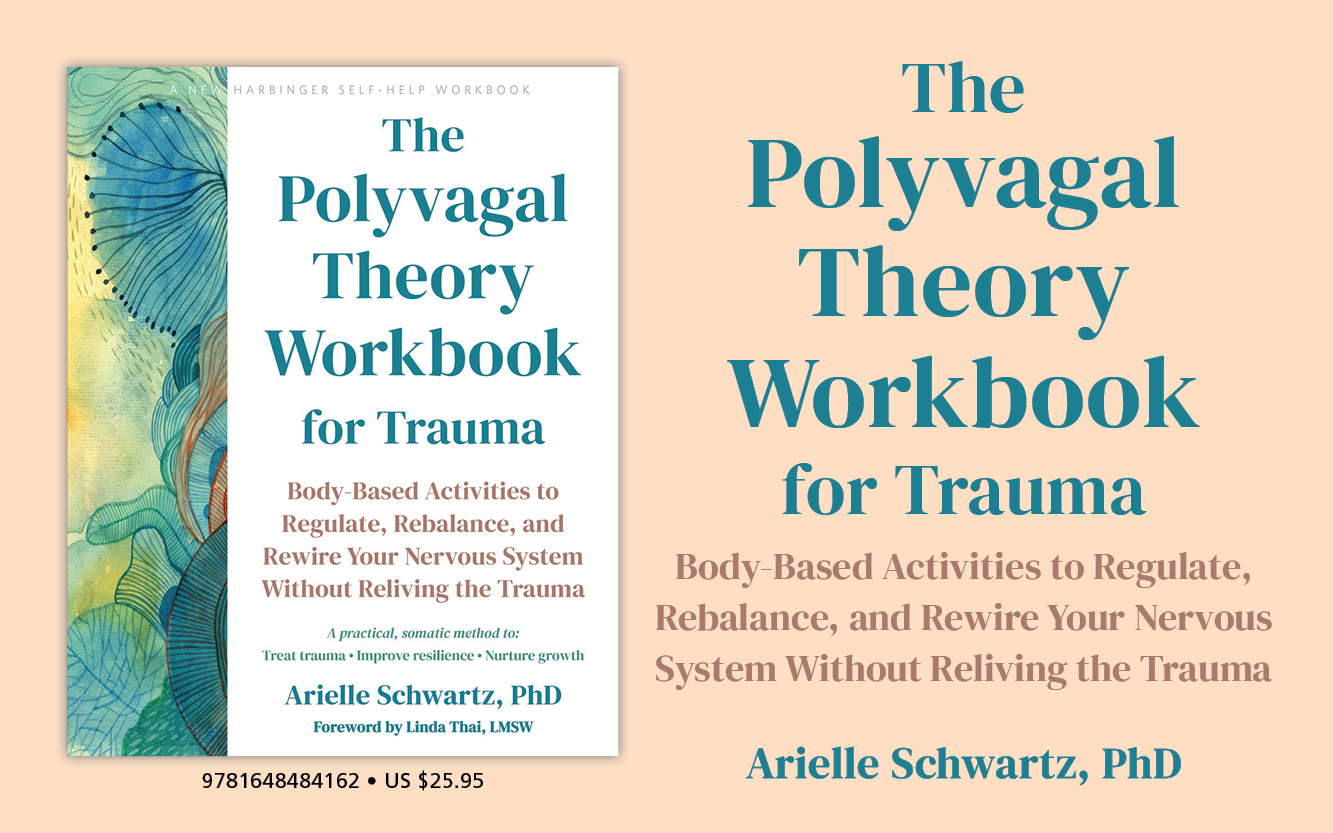
Body-Based Activities to Regulate, Rebalance, and Rewire Your Nervous System Without Reliving Your Trauma “In The Polyvagal Theory Workbook for Trauma, Arielle Schwartz gives you practical,

A Mind-Body Approach to Care Traumatic events can leave you feeling broken or disconnected. In order to survive, we often disconnect from painful emotions and
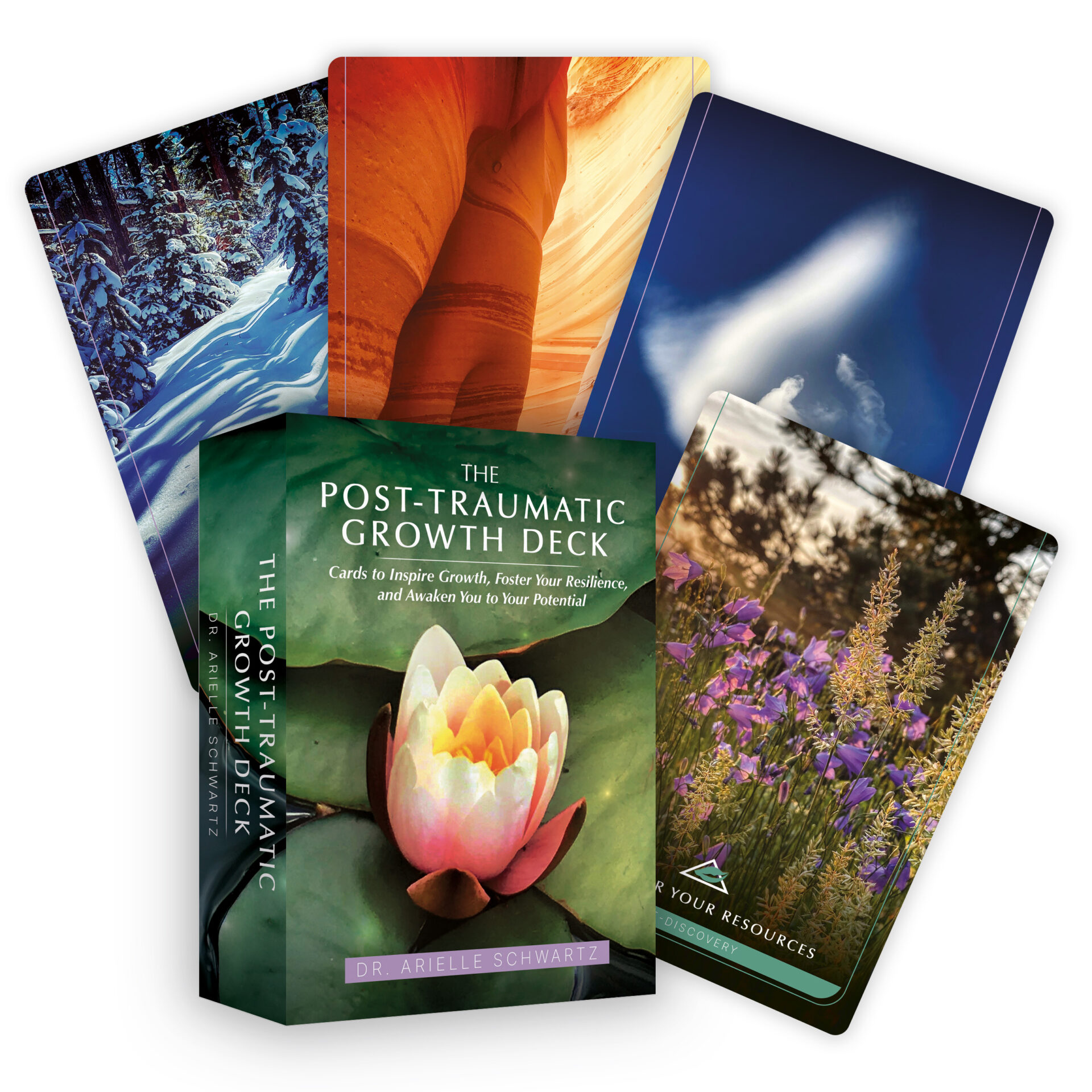
Cards to Inspire Growth, Foster Resilience, and Awaken Potential Within the Post-Traumatic Growth Deck, Dr. Arielle Schwartz integrates her love of photography with her passion

Support for your Healing Journey One of the most common barriers to healing that I see as a psychologist and trauma specialist is when we

In-Person Retreat September 19th – 21st, 2025 Trauma affects the best of us, and its effects can linger, limiting your ability to live with joy

A Poetic Soul Bath In this post, I share with you a poem called “For Now We are Free” that I wrote after the Polyvagal
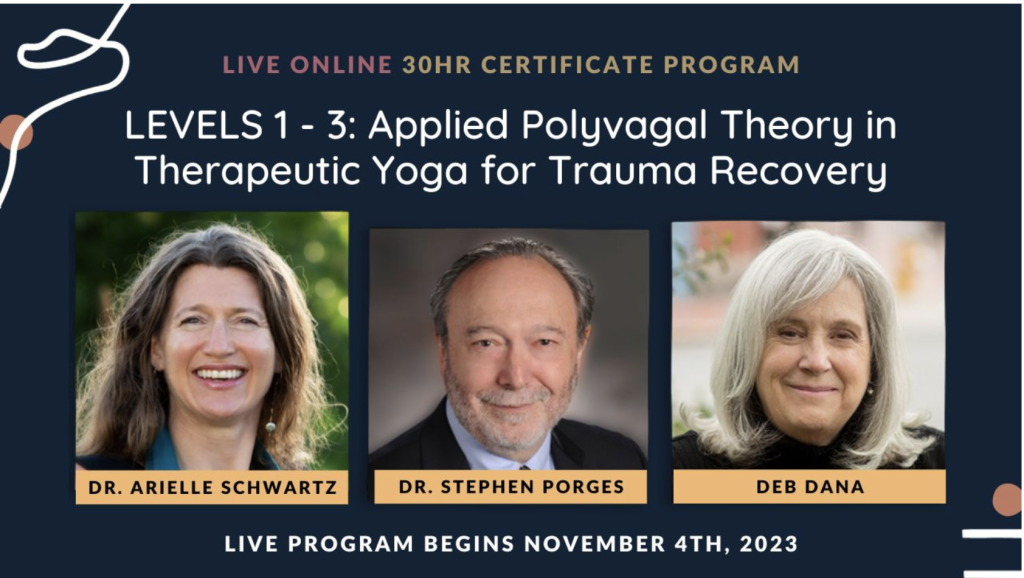
30-Hour Certification with The Embody Lab You are invited to step into a journey of empowerment, to learn the power of Applied Polyvagal Theory in